Each year, approximately 700,000 people have a heart attack. Heart attack survivors are at an increased risk for recurrent heart attacks and sudden cardiac death. Cardiac rehabilitation is very beneficial in heart disease.
Cardiac Rehabilitation in Heart Disease
We know that the heart is a muscle and muscle responds to exercise. Often times, when people have a heart attack or any other kind of heart disease, they tend to lose confidence in their exercise ability.
One of the greatest benefits of cardiac rehabilitation in heart disease is the ability to restore someone’s self-confidence. Cardiac rehabilitation in heart disease also restores confidence.
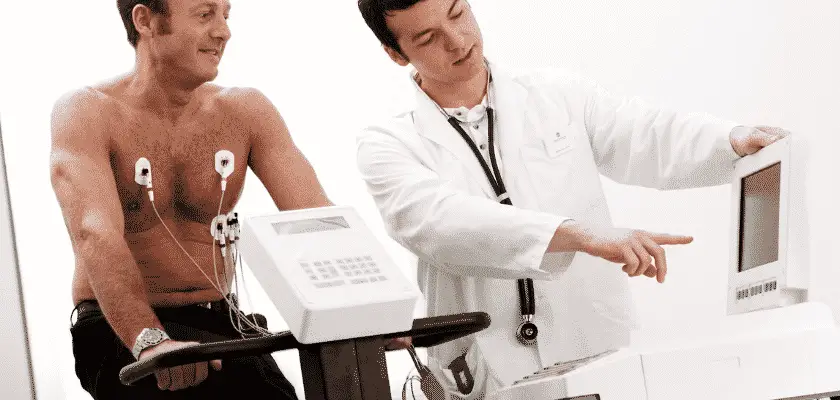
When you are in a cardiac rehabilitation program, you are typically monitored by nurses or other health care professionals. You are attached to a heart monitor and your heart rate and blood pressure are monitored.
This article will be discussing inpatient rehab. Home outpatient rehab is also available through home health agencies.

Phases of Cardiac Rehabilitation Physical Therapy
Although cardiac rehab has been associated with improved quality of life and survival rates, the majority of people do not participate in cardiac rehab. There are 3 phases in cardiac rehabilitation.
Cardiac rehabilitation typically involves four phases, each focused on different aspects of recovery and promoting overall cardiovascular health. The four phases are as follows:
- Phase 1: Inpatient/Immediate Postoperative Phase This phase starts immediately after cardiac surgery or a cardiac event, while the patient is still in the hospital. The primary goals of this phase are to monitor the patient’s vital signs, manage pain, promote early mobilization, and provide education about the upcoming phases of cardiac rehabilitation. Medical professionals closely supervise the patient’s progress and ensure a safe transition to the next phase.
- Phase 2: Early Outpatient Phase 2 begins once the patient is discharged from the hospital and continues for several weeks. It focuses on gradually increasing the patient’s exercise capacity and overall physical activity level. The program includes supervised exercise sessions, education on heart-healthy lifestyle modifications, dietary counseling, and emotional support. The exercises are tailored to the patient’s individual needs and may include aerobic exercises, resistance training, and flexibility exercises.
- Phase 3: Intensive Outpatient Phase 3 builds upon the progress made in Phase 2 and aims to further improve cardiovascular fitness, endurance, and strength. This phase typically lasts for several months and involves structured exercise sessions held in a cardiac rehabilitation center or under the supervision of a healthcare professional. The patient learns more advanced exercises, receives ongoing education on risk factor management, nutrition, stress reduction, and receives psychosocial support.
- Phase 4: Maintenance/Long-Term Phase 4 focuses on maintaining the gains achieved in the previous phases and sustaining a heart-healthy lifestyle in the long run. The patient transitions to independent exercise and self-monitoring, but may still participate in supervised exercise sessions periodically. This phase emphasizes long-term adherence to regular physical activity, healthy eating habits, and lifestyle changes to reduce the risk of future cardiac events.

It is important to note that the structure and duration of each phase may vary depending on the individual’s specific needs, medical condition, and healthcare provider’s recommendations.
The focus was on bed rest and avoidance of stress. Heart attack patients were placed on six weeks of bed rest. In 1950, the concept of cardiac rehab was originated. With the invention of more sophisticated coronary care units, cardiac rehab began.
Admission into a Cardiac Rehab Program
- Referral: The first step is to receive a referral from a healthcare professional, usually a cardiologist, cardiac surgeon, or primary care physician. They will assess your medical condition and determine if you are a suitable candidate for cardiac rehabilitation. Common indications for referral include recent heart surgery (such as coronary artery bypass grafting or valve replacement), heart attack, stable angina, or other cardiovascular conditions.
- Medical Evaluation: Once referred, you will undergo a comprehensive medical evaluation. This evaluation aims to assess your overall health status, identify any specific cardiac risk factors, and determine your exercise capacity. It may involve physical examinations, medical history review, blood tests, electrocardiogram (ECG/EKG), stress tests, echocardiography, or other diagnostic tests as needed.
- Assessment and Goal Setting: Based on the medical evaluation, a team of healthcare professionals, including doctors, nurses, exercise specialists, and dietitians, will work with you to develop an individualized cardiac rehabilitation plan. They will set specific goals tailored to your needs, taking into account your medical history, exercise tolerance, and personal preferences.
- Program Enrollment: Once the assessment and goal setting are completed, you will be enrolled in a cardiac rehabilitation program. These programs are often conducted in specialized centers or hospitals, although some may also be offered in community settings or through home-based programs. You will be provided with a schedule for your sessions and given any necessary instructions or materials.
- Cardiac Rehabilitation Sessions: The actual cardiac rehabilitation sessions will typically involve a combination of supervised exercise, education, counseling, and support. Exercise sessions are designed to gradually improve your cardiovascular fitness, strength, and endurance. Educational components may cover topics such as heart-healthy lifestyle modifications, medication management, stress reduction, and dietary guidelines. Counseling and support can address emotional well-being, coping strategies, and risk factor management.
- Ongoing Monitoring and Progress Evaluation: Throughout the program, your progress will be regularly monitored and evaluated by the healthcare team. This may involve periodic reassessments of your exercise capacity, measurements of blood pressure, heart rate, and weight, as well as ongoing discussions about your overall well-being. The program may be adjusted based on your progress and any changes in your medical condition.
It’s important to remember that the specific details and duration of a cardiac rehabilitation program can vary depending on individual circumstances and healthcare provider preferences. Your healthcare team will guide you through the entire process, ensuring that you receive appropriate care and support to aid in your cardiac recovery and improve your long-term cardiovascular health.

What is Cardiac Rehab Program: Risk Reduction Strategies
Cardiac rehabilitation includes:
- Exercising and physical training
- Nutritional counseling
- Smoking cessation
- Diabetes
- Psychosocial intervention
- Management of lipid levels and long-term management
Who Should get Cardiac Rehab?
- Patients with Acute Coronary Syndrome
- ST elevation heart attacks
- Newly diagnosed heart failure, and chronic heart failure with a change
- Patients with heart transplants and LVAD
- Patients who have had ICD insertions
- Patients with exertional chest pain, and
- Patients with heart valve replacements
Will Insurance Cover Cardiac Rehab?
Participation in cardiac rehab ranges from 20% to 50%. Some of the barriers to patients not participating in cardiac rehab are physician’s reluctance to refer some patients to rehab. Women, minorities, and patients from lower socioeconomic levels are also not referred to cardiac rehab.
Medicare Part B covers comprehensive cardiac rehab. You must be referred by your doctor and have had any of the following:
- A heart attack in the last 12 months
- Coronary artery bypass surgery
- Current stable angina pectoris
- A heart valve repair or replacement
- A coronary angioplasty or coronary stent
- A heart or heart-lung transplant
- Stable chronic heart failure
Phase III is also called the maintenance program. This is a supervised but non-monitored program that also takes place within the Cardiac Rehabilitation department. Patients remain in this program for various lengths of time depending on physician recommendation as well as each patient’s needs and goals. When patients complete Phase III, they are given home exercise guidelines to follow.
Cardiac Rehabilitation Program At Home
Medicare and some private insurances will pay for rehab services at home. According to this study, “Home-based programs have been developed to provide nurse-led, community-based, self-help programs for patients who may not be able to repeatedly attend hospital-based programs.
With the increasing financial burden of coronary heart disease worldwide, the development of an affordable, acceptable and appropriate method of community-based cardiac rehabilitation is of significant importance”
Bottom Line:
Cardiac rehabilitation has great benefits for the heart patient. Its benefits have been proven. What has been your experience with cardiac rehab? Cardiac rehabilitation in heart disease has been proven to help patients overcome their fears.
References
https://pubmed.ncbi.nlm.nih.gov/30725881/
My name is Phyllis Robinson MSN, RN. I have been a Registered Nurse for 27 years in the Cardiac Intensive Care Unit. I am passionate about cardiac care and heart disease. I also want this blog to be an educational tool that people can refer to for traditional and alternative treatment. I will blog on heart disorders such as high blood pressure, congestive heart failure, cardiomyopathy, and high cholesterol.
I received my Nursing degree from Baltimore Community College.
I went on to receive my Masters in Nursing from Walden University
I have worked for almost 30 years in Critical Care with a focus on heart health. I am an advocate of preventive healthcare.




This a very informative. Great blog by the way.