Unveiling the Silent Killer: Understanding the Common Causes of Congestive Heart Failure
Welcome to a journey of uncovering the silent killer that claims the lives of millions worldwide – congestive heart failure.
In this eye-opening exploration, we will delve into the common causes of this debilitating condition and shed light on the alarming prevalence it holds in our society.
From lifestyle choices to underlying health conditions, we will unravel the intricate web of factors that contribute to the onset of congestive heart failure, empowering you with knowledge to take charge of your heart health.
Brace yourself for a riveting ride as we navigate through the maze of symptoms, risk factors, and preventive measures that can make all the difference in preserving your heart’s vitality.
Whether you are seeking to understand the warning signs, support a loved one, or simply expand your knowledge on this critical health issue, this captivating journey will equip you with the insights you need to protect your heart and embrace a healthier, more fulfilling life.

Common Causes of Congestive Heart Failure
Congestive heart failure can stem from a variety of causes, each contributing to the strain on the heart and its ability to pump blood effectively.
Understanding these causes is crucial in identifying potential risk factors and taking preventive measures.
Related Articles
The Link Between Sleep Apnea and Congestive Heart Failure
Can spicy food increase your heart rate?
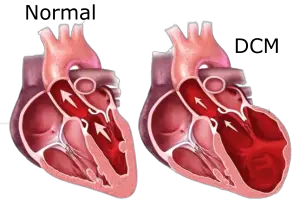
DCM Life Expectancy
Blood pressure chart 150/90
Essential oil for stroke prevention
One common cause of congestive heart failure is age.
As we grow older, our heart muscle naturally weakens, making it more susceptible to damage and impairing its ability to function optimally.
Additionally, lifestyle factors such as poor diet, lack of exercise, and excessive alcohol consumption can significantly increase the risk of developing congestive heart failure.
Another significant cause of congestive heart failure is underlying medical conditions.
Individuals with a history of coronary artery disease, high blood pressure, or diabetes are at a higher risk of developing congestive heart failure.
These conditions put extra strain on the heart, gradually weakening it over time.

Furthermore, certain medications and substances, such as chemotherapy drugs and excessive use of non-steroidal anti-inflammatory drugs (NSAIDs), can also contribute to the development of congestive heart failure.
While some cases of congestive heart failure are attributed to lifestyle and environmental factors, others are linked to genetic factors and congenital heart defects.
Certain individuals may be born with structural abnormalities in their hearts that increase the risk of heart failure later in life.
Genetic factors can also play a role in the development of heart disease, making some individuals more predisposed to congestive heart failure than others.
Age as a Leading Cause
The heart muscle gradually weakens, leading to a decreased cardiac output and an increased risk of heart failure.
This age-related decline in heart function is often accompanied by other factors, such as the accumulation of plaque in the arteries and the development of underlying medical conditions like high blood pressure and diabetes.
These factors further contribute to the strain on the heart, making it more susceptible to congestive heart failure.
It is important to note that while age is a significant risk factor for congestive heart failure, it does not mean that heart failure is an inevitable consequence of getting older.
By adopting a heart-healthy lifestyle and managing underlying medical conditions, individuals can mitigate the impact of age on their heart health and reduce their risk of developing congestive heart failure.

Lifestyle factors that contribute to congestive heart failure
Our lifestyle choices play a critical role in determining our heart health and can significantly contribute to the development of congestive heart failure.
Poor diet, lack of exercise, and excessive alcohol consumption are all lifestyle factors that can increase the risk of heart failure.
A diet high in saturated and trans fats along with eating high carbs, high Triglycerides and processed sodium can lead to the development of conditions such as high blood pressure, diabetes, and obesity, all of which are risk factors for congestive heart failure.
Additionally, a sedentary lifestyle devoid of regular physical activity can weaken the heart muscle and lead to the onset of congestive heart failure.
Engaging in regular exercise not only strengthens the heart but also helps control weight, reduce blood pressure, and improve overall cardiovascular health.
Excessive alcohol consumption is another lifestyle factor that can contribute to congestive heart failure.
Alcohol abuse can lead to hypertension, arrhythmias, and weakened heart muscle, all of which increase the risk of heart failure. Moderation is key when it comes to alcohol consumption, and individuals should strive to adhere to recommended guidelines to protect their heart health.
Medical conditions that can lead to congestive heart failure
Congestive heart failure often arises as a result of underlying medical conditions that put strain on the heart and gradually weaken it over time.
Coronary Artery Disease
One such condition is coronary artery disease, a condition characterized by the narrowing of the arteries that supply blood to the heart.
As the arteries become clogged with plaque, the heart muscle may not receive an adequate supply of oxygen-rich blood, leading to heart failure.
High Blood Pressure
High blood pressure, also known as hypertension, is another common medical condition that can lead to congestive heart failure.
Elevated blood pressure places increased strain on the heart, causing it to work harder to pump blood throughout the body.
Over time, this increased workload can weaken the heart muscle and ultimately result in heart failure.
Diabetes
Diabetes, a chronic condition characterized by high blood sugar levels, is also closely linked to congestive heart failure.
Uncontrolled diabetes can damage blood vessels and nerves in the heart, reducing its ability to function properly and increasing the risk of heart failure.
Valvular Heart Disease
Other medical conditions that can contribute to congestive heart failure include valvular heart disease, which affects the heart valves’ ability to regulate blood flow, and certain arrhythmias, which disrupt the heart’s normal rhythm and impair its pumping capacity.
Identifying and managing these underlying medical conditions is crucial in preventing or managing congestive heart failure.
The Importance of Vitamins and Minerals
Vitamins and minerals are essential nutrients that our bodies require to function properly. They play vital roles in various bodily processes, including energy production, immune function, and the maintenance of healthy heart function. Deficiencies in these nutrients can disrupt these processes and contribute to the development of health problems, including CHF.
Thiamine (Vitamin B1) and CHF
Thiamine is a crucial B-vitamin that helps convert food into energy and supports the proper functioning of the heart and nervous system. In the context of CHF, a deficiency in thiamine can lead to a condition known as “beriberi.” Beriberi can affect the cardiovascular system and cause symptoms such as fatigue, shortness of breath, and fluid retention, all of which are also common in CHF.
Magnesium and CHF
Magnesium is another essential mineral that plays a significant role in maintaining heart health. It helps regulate heart rhythm, blood pressure, and muscle function. A deficiency in magnesium can contribute to arrhythmias (irregular heartbeats) and increase the risk of cardiovascular issues, including CHF.
How Deficiencies Lead to CHF
When the body lacks adequate amounts of thiamine and magnesium, various mechanisms can contribute to the development of CHF:
- Energy Production: Both thiamine and magnesium are essential for the proper functioning of enzymes involved in energy production. Without enough of these nutrients, the heart muscle may not have the energy it needs to pump blood effectively.
- Heart Muscle Function: Magnesium is crucial for maintaining the proper contraction and relaxation of the heart muscle. A deficiency can lead to impaired heart muscle function and potentially weaken the heart’s pumping ability.
- Fluid Balance: Thiamine and magnesium deficiencies can disrupt fluid balance in the body, leading to fluid retention and swelling, which are common symptoms of CHF.
Prevention and Management
To prevent deficiencies and reduce the risk of CHF:
- Maintain a balanced diet rich in a variety of nutrient-dense foods, including proteins, some fruits, and vegetables.
- Include sources of thiamine (whole grains, lean pork, legumes) and magnesium (nuts, seeds, leafy greens) in your diet.
- If you have concerns about your nutrient intake, consider consulting a healthcare professional or registered dietitian.
Medications and substances that may cause congestive heart failure
While medications and substances are intended to help treat various health conditions, some can inadvertently contribute to the development of congestive heart failure.
Certain chemotherapy drugs, such as anthracyclines, can have cardiotoxic effects, damaging the heart muscle and impairing its ability to pump blood effectively.
Individuals undergoing cancer treatment should closely monitor their heart health and discuss any concerns with their healthcare provider.
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs (NSAIDs), commonly used to alleviate pain and reduce inflammation, can also increase the risk of congestive heart failure when used excessively or over a prolonged period.
NSAIDs can cause sodium and water retention, leading to fluid buildup in the body and putting strain on the heart.
Recreational Drugs
Furthermore, recreational drugs such as cocaine and amphetamines can have detrimental effects on the heart and contribute to the onset of congestive heart failure.
These substances can cause blood vessels to constrict, elevate heart rate and blood pressure, and damage the heart muscle, increasing the risk of heart failure.
It is essential to be aware of the potential side effects of medications and substances and to consult with healthcare professionals to ensure their safe and appropriate use.

Genetic factors
While lifestyle choices and underlying medical conditions play a significant role in the development of congestive heart failure, genetic factors and congenital heart defects also contribute to the prevalence of this condition.
Some individuals may be born with structural abnormalities in their hearts, making them more susceptible to heart failure later in life.
Congenital Heart Defects
Congenital heart defects are structural abnormalities present at birth and can affect the heart’s valves, walls, or blood vessels.
These defects can disrupt the heart’s normal functioning, leading to heart failure or increasing the risk of developing heart failure in the future.
Early detection, proper management, and specialized care are crucial for individuals with congenital heart defects to minimize the risk of heart failure as they grow older.
Genetic Factors
Genetic factors can also influence an individual’s predisposition to heart disease and congestive heart failure.
Certain gene variations can affect how the heart functions and increase the risk of developing heart failure.
Understanding one’s genetic predisposition and family history can help individuals take proactive steps in managing their heart health and reducing their risk of heart failure.
Regular monitoring of blood pressure and routine check-ups with healthcare professionals are essential in managing hypertension and preventing complications such as congestive heart failure.

Recognizing the early signs and symptoms of congestive heart failure
Recognizing the early signs and symptoms of congestive heart failure is vital in seeking timely medical attention and preventing further deterioration of heart function.
While symptoms can vary from person to person, common signs of congestive heart failure include fatigue, shortness of breath, swollen ankles or feet, rapid or irregular heartbeat, persistent cough, and difficulty lying flat without experiencing shortness of breath.
Early symptoms of congestive heart failure may be subtle and easily attributed to other causes, such as aging or lifestyle factors.
However, it is crucial not to dismiss these symptoms and to consult with a healthcare professional for a comprehensive evaluation.
Prompt diagnosis and treatment can help manage congestive heart failure and improve overall quality of life.
Underlying Medical Conditions
Individuals who have a history of underlying medical conditions, such as coronary artery disease, high blood pressure, or diabetes, should be particularly vigilant in monitoring their heart health and reporting any new or worsening symptoms to their healthcare providers.
Regular check-ups and recommended screening tests can aid in the early detection of heart-related issues and the implementation of appropriate preventive measures.
Prevention and management strategies for congestive heart failure
Prevention and management of congestive heart failure require a multidimensional approach that encompasses lifestyle modifications, proper management of underlying medical conditions, and adherence to prescribed medications.
Adopting a heart-healthy lifestyle is crucial in reducing the risk of developing congestive heart failure.
Importance of a Balanced Diet
A balanced diet rich in fruits, vegetables, whole grains, proteins, and healthy fats can help maintain a healthy heart and prevent the onset of heart failure.
Regular physical activity, such as aerobic exercises, can strengthen the heart muscle and improve cardiovascular health.
Avoiding tobacco use and excessive alcohol consumption are also essential in preserving heart health.
Managing underlying medical conditions, such as high blood pressure, diabetes, and cholesterol, is vital in preventing or managing congestive heart failure.
This may involve taking prescribed medications, monitoring blood pressure and blood sugar levels, and making lifestyle modifications to control these conditions effectively.
Importance of Having Regular Checkup
Regular check-ups with healthcare professionals, including cardiologists, can aid in the early detection and management of heart-related issues. These professionals can provide guidance on preventive measures, recommend appropriate screenings, and adjust treatment plans as needed.
Conclusion
In conclusion, congestive heart failure is a serious condition that requires awareness, prevention, and management.
By understanding the common causes of congestive heart failure, recognizing the early signs and symptoms, and implementing preventive strategies, individuals can take charge of their heart health and embrace a healthier, more fulfilling life.
Promoting heart health is a collective effort that requires education, support, and proactive measures to combat the silent killer that is congestive heart failure.
Let us join hands in raising awareness, supporting research, and prioritizing heart health to protect our most vital organ – the heart.
References
https://pubmed.ncbi.nlm.nih.gov/9008688/
My name is Phyllis Robinson MSN, RN. I have been a Registered Nurse for 27 years in the Cardiac Intensive Care Unit. I am passionate about cardiac care and heart disease. I also want this blog to be an educational tool that people can refer to for traditional and alternative treatment. I will blog on heart disorders such as high blood pressure, congestive heart failure, cardiomyopathy, and high cholesterol.
I received my Nursing degree from Baltimore Community College.
I went on to receive my Masters in Nursing from Walden University
I have worked for almost 30 years in Critical Care with a focus on heart health. I am an advocate of preventive healthcare.