Sarcoidosis
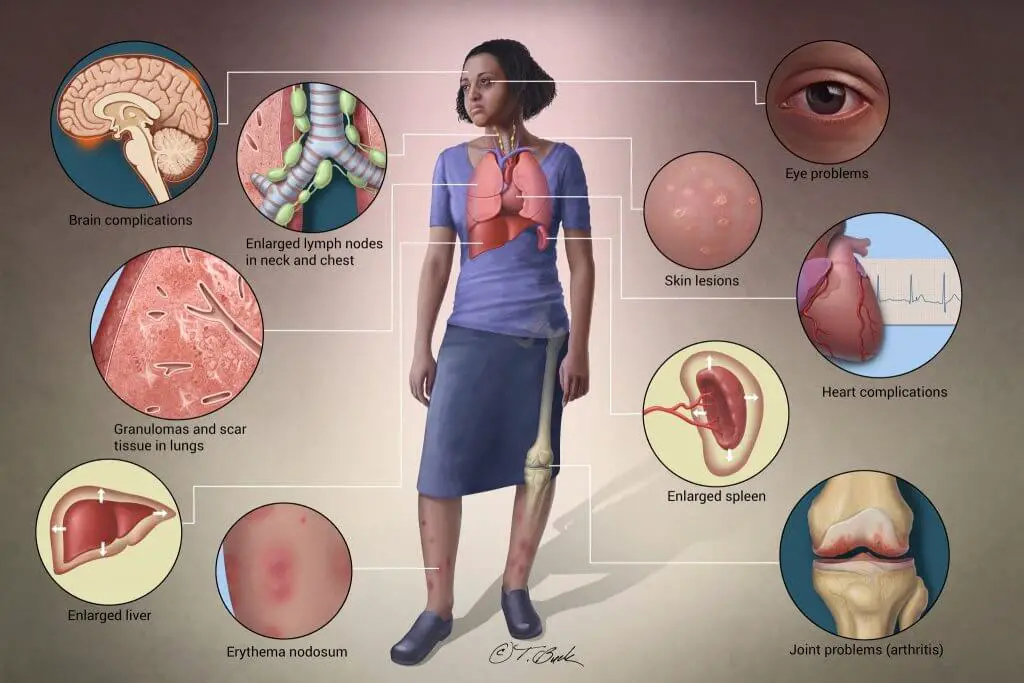
Sarcoidosis is an inflammatory disease that can affect any organ. However, the most devastating organs that are affected are the lungs, heart, and kidneys.
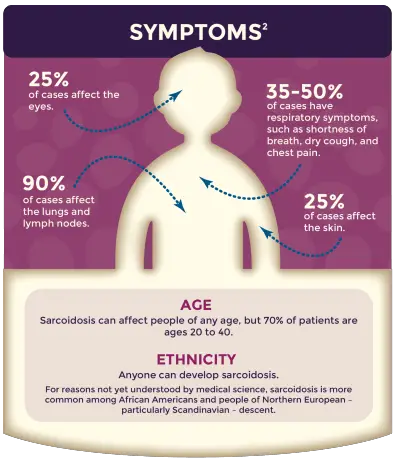
Ninety percent of the time, sarcoidosis affects the lungs.
Sarcoidosis affects people from all around the world. This disease commonly affects people between the ages of 20 and 40. Women are more affected than men.
The highest incidence of granulomas has been observed in Northern European countries. There are also high occurrences in Japan and the United States.
African Americans are far more likely than White Americans to contract sarcoidosis. African American women are the most commonly affected group. In African Americans, sarcoidosis usually involves several organs, and it leads to death more than any other group.
How Does Sarcoidosis Develop?
Sarcoidosis is thought to develop when there is a defect in the immune system. Some of the suggested causes of sarcoidosis are:
- An unidentified toxic substance
- An unknown environmental cause
- A viral or bacterial infection
These theories have really taken on a new meaning in the wake of the 9-11 terror attacks when first responders have contracted several lung disorders including sarcoidosis and cancer.
Organs That Are Affected by Sarcoidosis
Lungs:
The lungs are the most commonly affected organ in sarcoidosis. Ninety percent or more of people with sarcoidosis have lung involvement, whether they have symptoms or not. Symptoms specific to sarcoidosis affecting the lungs include:
- Dry coughing
- Trouble breathing, wheezing, or pain with breathing
- Chest pain, tightness, or discomfort
- Coughing up blood (which is rare), especially in the early stages of sarcoidosis.
There are many problems that can be caused by sarcoidosis affecting the lungs, usually only in the most serious cases. Those problems include:
- Pulmonary Fibrosis: scarring that occurs in the lungs as a result of untreated or unyielding inflammation/granuloma formation. As scar tissue builds up in the walls of air sacs in the lungs, it can make it hard for oxygen to get into your blood over time, leading to reduced oxygen levels in the blood and shortness of breath. Pulmonary fibrosis belongs to a larger group of lung diseases called “interstitial lung diseases,” another way in which your doctor might refer to your condition.
- Fibrocystic disease: an advanced form of lung disease in which scars block airways in one or both lungs
- Pulmonary hypertension: a condition in which scar tissue narrows or blocks arteries in the lungs, causing high blood pressure. The high blood pressure, also known as hypertension, forces the heart to work harder to pump blood through the vessels. Over time, heart muscle builds up and weakens, hindering its ability to deliver oxygen to lungs and other parts of the body.
- Bronchiectasis: a condition in which the walls of the bronchi, or airways in the lungs, thicken due to chronic inflammation/granuloma formation. Over time, bronchi become unable to clear out mucus. The mucus then builds up, creating an environment where bacteria will grow. Over time, the airways become inflamed, stretched out, and scarred, making it harder for the lungs to move air through them.
- Aspergilloma: a clump of fungus that forms in healed lung scars and enlarged airways, and can cause bleeding in the lungs.
Sourced from https://www.stopsarcoidosis.org/what-is-sarcoidosis/organs-involved/
Skin
Roughly a quarter of people with sarcoidosis will develop skin problems related to the disease. Often, these skin problems can indicate the seriousness of the case of sarcoidosis.
Skin problems might include:
- Erythema nodosum, which causes raised, red, and tender bumps to form on the skin, usually on the front of the legs. Nearby joints are often swollen and painful. Erythema nodosum usually goes away on its own in six to eight weeks, even without treatment. Often, the presence of erythema nodosum is a good sign, indicating the type of sarcoidosis that also goes away on its own after a few months or years.
- Lupus pernio, which is an uncommon skin condition that causes hard, reddish-purplish bumps to form on the cheeks, nose, lips, and/or ears. These bumps do not go away on their own and often come back when treatment is stopped. They are usually associated with chronic sarcoidosis. In some cases, the sores are disfiguring and can damage underlying cartilage and bone.
- Other bumps on or under the skin, rashes, sores, scaling, and/or changes in old scars or tattoos that do not go away and are rarely painful or itchy. These skin problems are associated with the kind of sarcoidosis that lasts a long time.
Heart
Researchers estimate that sarcoidosis of the heart, or cardiac sarcoidosis, affects more than 10 percent of people with sarcoidosis in the United States, and perhaps as many as 25 percent. Because heart problems can be very serious, everyone who has sarcoidosis should be screened for cardiac sarcoidosis.
Some people with heart involvement might notice symptoms, but many people will feel no obvious effect, even in late-stage disease.
Heart symptoms might include:
- Irregular heartbeats, which can feel like palpitations and/or skipped beats
- Shortness of breath, coughing, chest tightness, and/or wheezing (although these symptoms can also be associated with lung problems)
- Swelling in the legs, which usually occurs only in late-stage sarcoidosis of
the heart - Feeling lightheaded or fainting
- Heart attack
The problems caused by cardiac sarcoidosis can include:
- Arrhythmias, which are abnormal heartbeats or rhythms.
- Heart blocks, which are the blockage of electrical impulses that regulate the heart rate, impairing blood flow to the rest of the body.
- Heart failure, which occurs when the heart is unable to pump enough blood through the body, causing blood and fluid to back up in the lungs and elsewhere.
- Pericarditis, which although rare, can cause inflammation of the covering of the heart, as well as chest pain.
- Heart valve problems, which can prevent blood from flowing through the heart correctly.
- Heart attacks, which can occur when a blockage prevents blood and oxygen from reaching part of the heart.
How is Sarcoidosis Diagnosed? Being Diagnosed With Sarcoidosis
Sarcoidosis is diagnosed by biopsy. The clumps of inflammatory cells are called granulomas.
When the body recognizes a foreign object, the body responds with cells called granulomas.
Sarcoidosis is thought to be caused by environmental toxins.
Before a person has a biopsy, there are other diagnostic tests that must be done. Often times, a person is diagnosed by routine checkups such as an X-ray or a CT scan. Sometimes the person doesn’t have any symptoms. These scans usually show enlarged lymph nodes.
This disease is tricky because some people do not any treatment, and some people require immediate treatment that can last for years.
Treatment Options
- Corticosteroids: Corticosteroids reduce inflammation. They are not the same as anabolic steroids, the type of steroid that is sometimes abused by athletes. Corticosteroids are the primary treatment for sarcoidosis. Treatment with corticosteroids relieves symptoms in most people within a few months. The most commonly used corticosteroids are prednisone and prednisolone. People with sarcoidosis may need to take corticosteroids for many months. Because these medications can cause side effects (including weight gain, insomnia, mood swings, acne, difficulty regulating blood sugar, and bone loss), your health care provider will gradually decrease your dose of medication after you start to take it.
- Immune system suppressant medication: Because sarcoidosis may be the result of an overreaction of the immune system, suppressing the immune system may ease symptoms and prevent further organ damage. When corticosteroids are not effective, your provider may talk with you about starting other medications, including methotrexate, azathioprine, and mycophenolate mofetil (CellCept). Other medications may help a few patients who do not respond to other therapies. They may include cyclophosphamide and biologic response modifiers (biologics or TNF-blockers).
- Antimalarial drugs: These medications were originally used (and are still used) to treat malaria. As a treatment for sarcoidosis, these drugs are most likely to be effective in people who have skin symptoms or a high level of calcium in their blood. Hydroxychloroquine (Plaquenil) and chloroquine (Aralen) are antimalarial drugs that are used to treat sarcoidosis. Both can cause stomach irritation and eye problems.
People with severe or advanced lung sarcoidosis may need oxygen therapy. In a few cases, lung transplantation – the replacement of a diseased lung or lungs with a healthy donor lung – is used to treat severe lung sarcoidosis.
https://www.stopsarcoidosis.org/what-is-sarcoidosis/treatment-options/
Nurse Musings
As a nurse with close to 30 years of experience, I have cared for many people diagnosed with sarcoidosis. The tricky thing about this disease is that it affects people in so many different ways.
It is so hard to predict the prognosis because people with sarcoid present differently. Some patients lungs are affected and others their kidneys are affected. Then some have cardiac sarcoid involvement. Patients with lung and heart involvement have a more challenging prognosis.
The most important things that patients can do is to maintain their appointments and to take their medications.
References:
Wu JJ, Schiff KR. Sarcoidosis. Am Fam Physician. 2004;70(2):312–322.
Baughman RP, Teirstein AS, Judson MA, et al.; Case Control Etiologic Study of Sarcoidosis (ACCESS) research group. Clinical characteristics of patients in a case-control study of sarcoidosis.Am J Respir Crit Care Med. 2001;164(10 pt 1)