Therapeutic hypothermia protocol saves the brain after a cardiac arrest or heart attack. Decreasing the temperature helps brain injuries after a cardiac arrest. There are a plethora of reasons for someone to sustain a brain injury. In this article, we will discuss brain injuries that result from a person’s cardiac arrest. When people have a sudden cardiac arrest, or when a person has a witnessed cardiac arrest, they are a candidate for a protocol that is called the Hypothermia Protocol.
Philips Medical Systems M5066A-CO2 Onsite AED with Slim Carry Case
What is the Hypothermia Protocol That Saves the Brain
Decreasing core temperature has been shown to improve survival rates and neurological status in people that have had an arrest from ventricular fibrillation or ventricular tachycardia. Usually, the protocol is started in the emergency department because that’s where the majority of the cardiac arrest patients come in.
They usually come in via 911. Once the emergency personnel is able to restart their heart, they will usually implement hypothermia protocol or decreased the core temperature. When the temperature is decreased, the brain does not need as many metabolic demands. This allows for the brain to heal.
There are some contraindications for this protocol. Such as :
- A pre-existing coma
- Sepsis
- Major surgery
- Active bleeding
- Traumatic head injuries
- Respiratory failure
Experts are not sure why cooling the body, reduces brain damage. Perhaps the chemical reactions of the body slow down and the Lord temperature may also lessen inflammation in the brain.
Immediate Post Arrest
1. Patients who meet inclusion criteria post-cardiac arrest should have their core body temperature reduced to 32° –
34°C as soon as possible, ideally within 4 hours of return of spontaneous circulation (ROSC).
2. If the patient is not already in an Intensive Care Unit (ICU) arrangements must be made to a transfer to the first
available ICU bed.
3. One to one nursing care is required for any patient receiving therapeutic hypothermia.
4. The patient’s circulation must be maintained with a Systolic B/P > 90mm/HG and airway with 02 saturation of
>90%.
5. The goal is to continue the therapeutic hypothermia for a period of 24 hours from initiation of cooling.
6. Once 24 hours of cooling has occurred, a slow (passive) rewarming phase will be initiated to reach the goal
temperature of 36.5° Celsius. It should happen no faster than an increase of 0.25°C per hour.
How Does the Hypothermia Protocol Work? How Long is the Protocol?
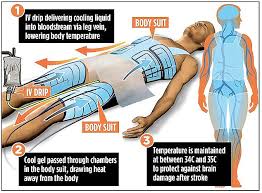
Once the patient has been resuscitated, the physicians will order a Hypothermia Protocol. The patient is actually cold for 24 hours to a goal temperature of 32- 34°C ) 89-93F). Back in the day, we used to just use cold saline and cooling blankets. However, we now have a machine made by Zoll that will automate the entire process.
This process should be started as soon as possible but no later than six hours after the patient has been resuscitated. Hypothermia temperature is maintained for 24 hours starting from the time of the initial therapy.
The rewarming phase begins at our 24. Protocol says that the body should not be reheated any faster than 0.5°C per hour until the normal temperature is reached. At this point, a normal temperature should also be maintained for another 24 hours.
Unlike the rewarming bees, the cooling phase must be done as rapidly as possible to achieve maximum effectiveness.
The effectiveness of the Hypothermia Protocol
Only one-third of patients admitted to the hospital survive to hospital discharge. Approximately one out of ten people who experience an out of hospital cardiac arrest survive to be discharged from the hospital. Only 2 out of 3 of them have a good neurologic recovery.
Every household who has a person with heart disease need to have an automatic defibrillator.
This is the training unit for the defibrillator.
This is an oxygen bag that is used for CPR.
These are the disposable masks to be used.
Conclusion
FAQ
Q: What is the hyperthermic protocol for cardiac arrest?
A: The hyperthermic protocol, also known as therapeutic hypothermia or targeted temperature management, is a medical treatment used after cardiac arrest. It involves lowering the body’s core temperature to a specific range (usually around 32-36 degrees Celsius or 89.6-96.8 degrees Fahrenheit) for a set period of time to minimize brain damage and improve chances of survival.
Q: How is the hyperthermic protocol performed?
A: The protocol typically involves using cooling devices, such as cooling blankets or intravascular cooling catheters, to cool the body. The patient is sedated and receives muscle relaxants to prevent shivering, as shivering can interfere with the cooling process. Once the desired temperature is reached, the patient is gradually rewarmed over a period of 24 to 48 hours.
Q: Why is the hyperthermic protocol used?
A: The protocol is used to reduce brain injury and improve neurological outcomes following cardiac arrest. Cooling the body slows down metabolism, decreases inflammation, and helps preserve brain function. It has been shown to improve survival rates and neurological recovery in some cases.
Q: When is the hyperthermic protocol initiated?
A: The protocol is typically initiated as soon as possible after resuscitation from cardiac arrest. The sooner it is started, the better the potential outcomes. However, it is important to note that not all patients who have experienced cardiac arrest are candidates for therapeutic hypothermia. The decision to use the protocol depends on various factors and should be made by medical professionals.
Q: Are there any risks or complications associated with the hyperthermic protocol? A: While the hyperthermic protocol is generally considered safe, there are potential risks and complications. These can include infections, bleeding, electrolyte imbalances, cardiac arrhythmias, and respiratory issues. The medical team closely monitors the patient during the entire process to minimize these risks.
Q: What happens after the hyperthermic protocol?
A: After the desired period of cooling and rewarming, the patient is gradually brought back to normal body temperature. Further supportive care and treatment are provided as needed. Rehabilitation and neurological assessment are crucial in the following days and weeks to evaluate the extent of brain injury and plan for appropriate care.