Updated 5/23/2023
Cardiac resynchronization therapy (CRT) is a procedure used to treat problems with how your heartbeats.
Cardiac Resynchronization is also called biventricular pacing. CRT is used to help with severe congestive heart failure.
It can also prevent atrial fibrillation. This article will discuss Cardiac Resynchronization Therapy (CRT): Overview, History, and Uses.
Cardiac Resynchronization Therapy (CRT): Overview, History, and Uses
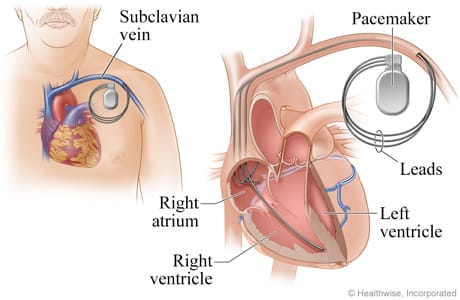
Your heart has two upper chambers called the atrium and two lower chambers called the ventricles. Your heart is synchronized when all areas of your heartbeat together.
When the areas of your heart do not beat as they should, your heart cannot pump enough blood and oxygen to your body.
You may have trouble breathing, tire easily, and have swelling in your feet and legs. Cardiac Resynchronization Therapy is indicated for patients with severe chronic heart failure.
This therapy has been proven to improve the quality of life for patients and prognosis.
The concept of CRT is to “make” the heart walls motion of the left ventricle be in synchronous with each other.
CRT has also been shown to prevent sudden cardiac death.
Related Articles
Can spicy food cause palpitations?
This is a video explaining in simple terms Cardiac Resynchronization
Cardiac Resynchronization Therapy: How to Prepare
- Write down the correct date, time, and location of your procedure
- Ask your caregiver if you need to stop using aspirin or any other prescribed medicine. Don’t forget to remind your doctor of any supplements or herbs you are taking.
- Bring your medication bottles, or bring a list of your medicines.
- You may need blood tests, EKG, Xray, etc before the procedure.
Cardiac Resynchronization Therapy: The Day of Your Procedure
- Ask your doctor if you should take any medication on the day of the procedure.
- You will be asked to sign a legal document called a consent form. This legal document should be read carefully because it explains what can go wrong during the procedure
- An anesthesiologist will come and talk to you before surgery. Make sure you let anesthesia know if you have ever had a reaction to anesthesia.
Cardiac Resynchronization Therapy: What Will Happen During the Procedure
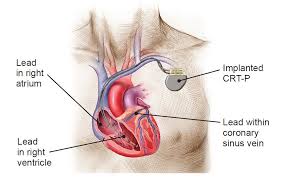
- A small incision is made over a vein near your neck. An electrode catheter holding three leads will be inserted through the incision. The catheter and leads are guided into your heart. One lead is placed in the right atrium, and one lead is placed into the left ventricle and one is placed in the right ventricle.
- If any of the leads cannot be placed through your vein, they may be placed through your chest. Three or four small cuts are made on your left side, between the ribs. The leads are placed directly on your heart. Once the leads are placed, a pacemaker is secured under the skin on your chest. The pacemaker will help your ventricles beat together and beat correctly with your right atrium. The doctor will close your incisions with stitches or medical glue.
Caring For Your New Device: CRT Precautions After Surgery
Patients are instructed to shower after 2 days, but the device should not get wet. After two weeks, most people are able to resume driving. Patients should only lift up to 10 pounds. Patients might have some soreness for up to 4-6 weeks.
Medtronic Devices has been testing a type of Cardiac Resynchronization Therapy devices called AdaptivCRT.
This device has been associated with improved patient survival. Medtronic did a study that included 1, 835 patients.
The use of this Cardiac Resynchronization Therapy (CRT) was associated with a 31% reduction in all-cause mortality compared to standard CRT.
According to Dr. Singh at the Massachusetts General Hospital, heart failure patients usually have other co-morbidities that they are dealing with. These conditions along with heart failure outs them at great risk for frequent hospitalizations, including death.
This AdaptivCRT has been shown to reduce hospitalizations, as well as the risk for atrial fibrillation.
Traditional CRT’s have standard settings, however, the AdaptivCRT device allows doctors to adjust the settings according to the patients’ needs.
When the settings are individualized, this resulted in a 59% in the reduction of the risk of patients getting admitted to the hospital with heart failure.
Heart failure affects more than 26 million people worldwide. Hopefully, this innovative technology will help prolong people’s lives.
FAQ
Q: What is Cardiac Resynchronization Therapy (CRT)? A: Cardiac Resynchronization Therapy (CRT) is a medical treatment for certain types of heart failure. It involves the implantation of a device called a CRT pacemaker or a CRT defibrillator (also known as a CRT-D) to help coordinate the pumping action of the heart’s chambers, known as ventricles. This therapy is also known as biventricular pacing.
Q: How does CRT work? A: CRT works by using an implanted device to deliver small electrical impulses to the heart muscle, which helps coordinate the contractions of the heart’s chambers. It typically involves pacing the right and left ventricles simultaneously, improving the synchronization of the heart’s pumping action. This helps to optimize the efficiency of the heart and improve its overall function.
Q: Who is a candidate for CRT? A: CRT is typically recommended for individuals with moderate to severe heart failure who have a specific type of abnormality in their heart’s electrical conduction system known as left bundle branch block (LBBB). It may also be considered for patients with certain other types of conduction abnormalities or in cases where drug therapy has not adequately improved symptoms.
Q: What are the benefits of CRT? A: The benefits of CRT include improved heart function, increased exercise capacity, reduced symptoms of heart failure (such as shortness of breath and fatigue), and a decreased risk of hospitalization. It can also improve the quality of life for individuals with heart failure.