When I am at work, whether I am working in the intensive care unit or the emergency department, we have to be prepared for all types of emergencies.
The 911- ambulance system has a way of communicating with the emergency department while in the field. This article will discuss stroke and atrial fibrillation with tPA.
What is Atrial Fibrillation?
Atrial fibrillation (AFib) is a type of cardiac arrhythmia, which is a condition where the heart’s rhythm becomes irregular.
In AFib, the heart’s upper chambers, called the atria, beat in a chaotic and disorganized manner, rather than the normal coordinated rhythm. This irregular and often rapid heartbeat can cause various symptoms and lead to complications.
Normally, the heart’s electrical signals start in the sinus node, a natural pacemaker located in the right atrium.
These signals then travel through the heart, causing it to contract and pump blood efficiently.
However, in atrial fibrillation, additional abnormal electrical signals arise, leading to irregular contractions of the atria.
The main characteristics of atrial fibrillation include:
-
Irregular heartbeat: The heart’s rhythm is irregular and can vary in speed, making it difficult to predict the pattern of the heartbeat.
-
Rapid heart rate: The heart may beat much faster than normal during AFib, causing palpitations or a sensation of a racing heart.

AFib is a common condition, especially in older adults, and it can be caused by various factors, including age, heart disease, high blood pressure, excessive alcohol consumption, thyroid problems, and other underlying medical conditions.
It’s important to diagnose and manage atrial fibrillation as it can lead to complications like blood clots, stroke, heart failure, and other cardiovascular issues.
Treatment options may include medications to control heart rate and rhythm, blood-thinning medications to reduce the risk of blood clots, and in some cases, procedures like cardioversion or catheter ablation to restore normal heart rhythm.
If you suspect you have atrial fibrillation or experience symptoms such as palpitations, shortness of breath, chest pain, or dizziness, it is essential to seek medical attention for proper evaluation and management.
What is a Stroke?
In the medical context, a stroke, also known as a cerebrovascular accident (CVA), is a serious medical condition that occurs when there is a sudden interruption or reduction of blood flow to the brain.
This lack of blood flow can be caused by either a blockage in a blood vessel (ischemic stroke) or the rupture of a blood vessel (hemorrhagic stroke).
Ischemic Stroke: This type of stroke is more common and happens when a blood clot or plaque buildup obstructs a blood vessel, cutting off blood supply to a specific area of the brain.
When a stroke occurs, the affected brain cells start to die rapidly due to the lack of oxygen and nutrients.
This can result in various neurological deficits, depending on which part of the brain is affected.
Common symptoms of a stroke include sudden weakness or numbness on one side of the body, difficulty speaking, vision problems, severe headache, and loss of balance or coordination.
Strokes are considered medical emergencies, and immediate medical attention is crucial to minimize brain damage and improve the chances of recovery.
Timely treatment with medications or medical procedures can help dissolve blood clots, reduce bleeding, and restore blood flow to the brain. Rehabilitation and ongoing care are often necessary to help patients recover and manage the consequences of a stroke.
An ischemic stroke is the only type of stroke that doctors use tPA. This is because an ischemic stroke is usually caused by a clot, and the tPA is a “clot buster”.
You would never give tPA to someone having a hemorrhagic stroke. This is because tPA is contraindicated in someone who is bleeding.
When a patient comes in with a sudden change in mental status, that is an emergency, and we need to scan the brain immediately. We need to ask questions such as:
How to Assess if A Person is Having a Stroke
- What was the patient doing?
- Has the patient been using drugs?
- How long has the pt had a change in mental status?
- What medications is the patient on?
- What is the patient’s previous medical history?
- Where did the patient come from?
When patients present with altered mental status, elevated blood pressure, irregular heartbeat, difficulty speaking, and motor weakness, the patient needs to be evaluated for a stroke. We see many patients with atrial fibrillation diagnosed with a stroke.
Related Articles
Pictures of Swollen Ankles Due to Congestive Heart Failure
Gift Ideas For Someone Who Has Had a Stroke
Why do Patients get a Stroke from Atrial Fibrillation (AFib)?
When you have atrial fibrillation, the normal rhythm of your heart becomes irregular, due to disorganized electrical signals in the atrium. This causes the upper chambers of your heart, called the atrium to beat irregularly.
This restricts blood from being efficiently pumped from your atrium to your ventricles. When your heart can‘t pump out blood effectively, the blood can clot and go up to your brain. This is called an ischemic stroke.
How are Stroke Patients Diagnosed
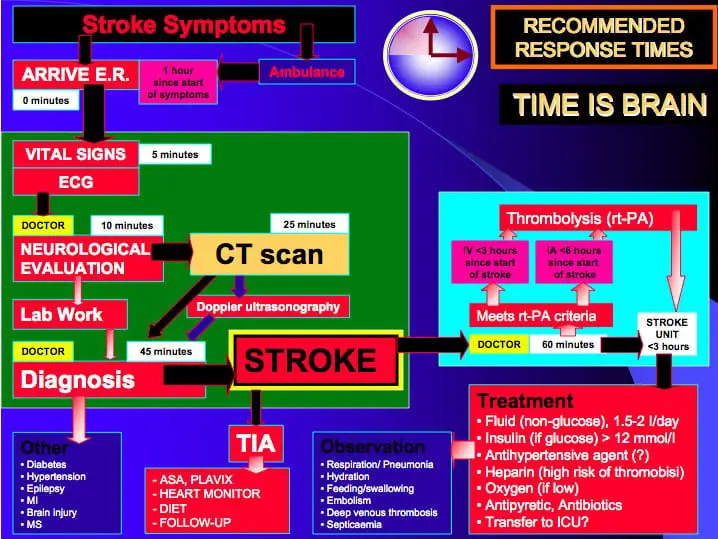
Cat Scan is the gold standard diagnostic test in the initial presentation to the hospital. Many times the Ct scan is negative. A follow-up test is almost always done with an MRI /MRA.
If the CT scan is positive, the patient will be considered for a clot-buster medication called Alteplase or tPA. However, there are some contraindications for when this medication can be given.
If the patient is already taking a blood thinner such as Xarelto, Coumadin, or Eliquis, they cannot receive tPA. If the patient presents with very high blood pressure, they cannot receive tPA.
A severe stroke, coma, or advanced age are contraindications to receiving tPA. Any recent hemorrhages, such as gastrointestinal bleeding, are contraindications. If the brain accident occurred more than 4 hours, the patient cannot get tPA.
- It is important to note that when patients start taking these blood thinners, it is extremely important to continue taking them, and don’t stop without your doctor’s consent. Many of these drugs, if suddenly stopped, will cause a stroke.
One of the main priorities is to figure out why the brain attack occurred. Patients will have a EKG, ECHO, or carotid duplex. The patient will most likely be admitted to the intensive care unit.
If the brain attack is thought to be from atrial fibrillation, the patient will be started on a blood thinner if there are no contraindications. The patient will also be started on medications to control the heart rate and rhythm.
Physical rehabilitation will be started immediately while in the hospital as evidence shows that the sooner rehab is started, the better the outcomes. If someone is exhibiting signs or symptoms of stroke you should call 911 immediately.
What is Tpa?
What is Activase?
Activase® (Alteplase), also known as t-PA, is a tissue plasminogen activator produced by recombinant DNA technology.
Activase belongs to the thrombolytic class of drugs and is the first drug to be indicated for the management of acute ischemic stroke.
All thrombolytic agents increase the risk of bleeding, including intracranial bleeding, and should be used only
in appropriate patients.
Not all patients with acute ischemic stroke will be eligible for Activase therapy, as defined by the following indication and contraindications.
Indications for tPA
Activase® (alteplase) is indicated for the treatment of acute ischemic stroke (AIS).
Exclude intracranial hemorrhage as the primary cause of stroke signs and symptoms prior to initiation of treatment.
Initiate treatment as soon as possible but within 3 hours after symptom onset.
Activase is indicated for use in acute myocardial infarction (AMI) for the reduction of mortality and reduction of the incidence of heart failure.
Limitation of Use: The risk of stroke may outweigh the benefit produced by thrombolytic therapy in patients whose AMI puts them at low risk for death or heart failure.
Activase is indicated for the lysis of acute massive pulmonary embolism (PE), defined as:
- Acute pulmonary emboli obstructing blood flow to a lobe or multiple lung segments.
- Acute pulmonary emboli accompanied by unstable hemodynamics, e.g., failure to maintain blood pressure without supportive measures.
Warnings and Precautions
Bleeding
Activase can cause significant, sometimes fatal internal or external bleeding, especially at arterial and venous puncture sites.
Avoid intramuscular injections and trauma to the patient. Perform venipunctures carefully and only as required.
Fatal cases of hemorrhage associated with traumatic intubation in patients administered Activase have been reported.
Natural Treatments
Although patients should continue to take their prescribed medications, there are some natural things that will help.
- Evidence has shown that low magnesium contributes to stroke.
- Consumption of fish and fish oils has been shown to decrease stroke incidence.
- A low-carb diet will reduce the incidence of stroke.
- A healthy weight and exercise will decrease the incidences of stroke.
Maintaining normal blood pressure is the best way to prevent a stroke.
Conclusion
In conclusion, a stroke is a serious medical condition that occurs when there is a sudden interruption or reduction of blood flow to the brain.
It can be caused by either a blockage in a blood vessel (ischemic stroke) or the rupture of a blood vessel (hemorrhagic stroke).
When a stroke happens, brain cells are deprived of oxygen and nutrients, leading to their rapid death and potentially causing various neurological deficits.
Prompt medical attention is critical in the event of a stroke to minimize brain damage and improve the chances of recovery.
Rehabilitation and ongoing care may be necessary for stroke survivors to manage the consequences of the condition.
It is essential to be aware of the warning signs of a stroke and seek immediate medical help if you suspect someone is experiencing one.


In 2015 my husband had a stroke due to his pre-existing a-fib condition. He didn’t show traditional symptoms like face drooping or slurred speech, he was able to give yes and no answers, but that was about all. I didn’t know what was going on (he had come home early from work while I was picking up our daughter from school) until his boss called and I overheard him ask Scott if he was home alone and he answered ‘yes’. I grabbed the phone and said that was wrong, and his boss told me to get him to the ER immediately, they thought he was having a stroke! When I told my husband to get in the car so we could go to the hospital and he agreed and went along easily, I KNEW something was most definitely wrong. Thankfully, it wasn’t as bad as the doctor’s first warned me, and he was able to go back to work in a few weeks. The effects were not all erased by speech and occupational therapy, but he’s a lot better off than losing all of his speech ability, as I was warned in the hospital.
Thank you for sharing this . I have also had a stroke. Thank God it was mild and I have word finding problems at times.