Updated 7/22/2023
I have been a bedside nurse for over 30 years and let me tell you the work is rewarding, but it can be exhausting!
Often times my legs are so sore and my joints are sore from walking on the cement floors.
The only saving grace for me is compression socks or stockings. We will discuss the best compression stockings for nurses and how to prevent varicose veins in nurses.
I have worn compression stockings since the beginning of my career. When nurses are on their feet all day, they are susceptible to varicose veins.
There are a couple of criteria that I use when I am buying compression socks.
- They have to be at least 15-20 mmHg
- And they have to be knee-highs


What Are Varicose Veins?
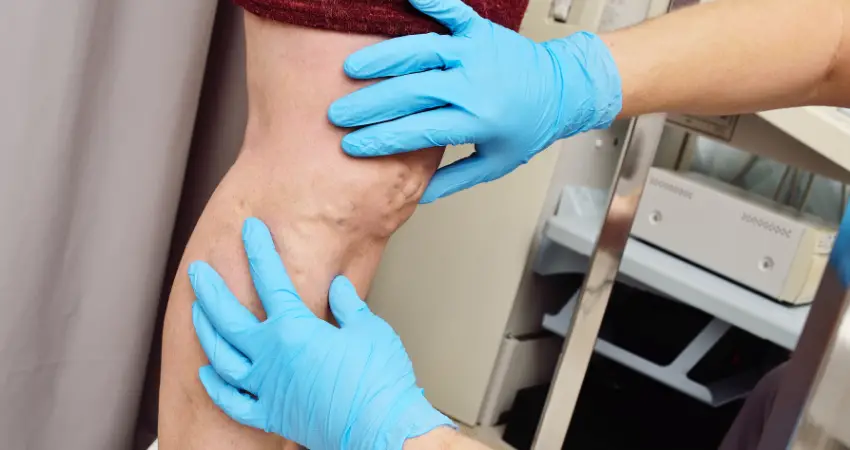
Varicose veins occur when a person’s veins become swollen and enlarged.
These veins are very uncomfortable and can cause pain. There are many remedies that people can use to help varicose veins.
The most simple remedy is to use compression stockings. Listed are the best compression stockings for nurses to prevent varicose veins. In this article, we will discuss the best compression socks for nurses.
Varicose veins are enlarged, swollen, and twisted veins that commonly appear in the legs and feet.
They occur when the one-way valves in the veins, which are responsible for pushing blood back up to the heart, become weak or damaged.

As a result, blood pools or accumulates in the veins, causing them to stretch and bulge.
The condition is more prevalent in the lower extremities because the veins in the legs have to work against gravity to return blood to the heart.
Symptoms of Varicose Veins in Nurses
Varicose veins can be dark purple or blue in color and are often visible just beneath the skin’s surface. They may also cause symptoms such as:
- Aching or throbbing pain in the legs.
- Swelling in the affected area.
- Itching or burning sensations.
- Muscle cramps or a feeling of heaviness in the legs.
- Discomfort worsened by prolonged standing or sitting.
- Unable to stand for 12 hour self
While varicose veins are generally not considered a severe medical condition, they can cause discomfort and cosmetic concerns for some individuals.
In more severe cases, they can lead to complications like skin ulcers or blood clots.
Factors that increase the risk of developing varicose veins include age, family history, being female, pregnancy, obesity, and a sedentary lifestyle.
Treatment Options For Varicose Veins
The treatment for varicose veins can vary depending on the severity of the condition and the individual’s specific symptoms.
Here are some common treatment options:
- Lifestyle Changes: Making certain lifestyle adjustments can help alleviate symptoms and prevent varicose veins from worsening.Regular exercise, especially activities that promote leg movement like walking or cycling, can improve blood circulation. Additionally, maintaining a healthy weight and elevating the legs when resting can reduce swelling and discomfort.
- Compression Stockings: Compression stockings are specially designed to provide pressure to the legs, helping to improve blood flow and reduce swelling. They can be beneficial in managing mild varicose veins and alleviating discomfort.
- Sclerotherapy: This non-surgical procedure involves injecting a solution directly into the affected veins. The solution irritates the vein walls, causing them to collapse and stick together. Over time, the treated veins are reabsorbed by the body, and blood is rerouted through healthier veins.
- Endovenous Laser Treatment (EVLT): EVLT is a minimally invasive procedure that uses laser energy to heat and seal the affected veins. This treatment is effective in closing off the damaged veins, redirecting blood flow to healthier ones.
- Radiofrequency Ablation (RFA): RFA is another minimally invasive procedure that uses radiofrequency energy to heat and seal varicose veins.
- Vein Stripping and Ligation: In more severe cases, surgical procedures like vein stripping and ligation may be recommended. Vein stripping involves removing the affected vein through small incisions, while ligation involves tying off the vein to prevent blood flow.
- Ambulatory Phlebectomy: This procedure involves making small incisions to remove smaller varicose veins close to the skin’s surface.

It’s essential to consult a qualified healthcare professional or a vascular specialist to determine the most appropriate treatment for individual cases.
The choice of treatment will depend on factors such as the size, location, and extent of the varicose veins, as well as the presence of any underlying health conditions.
Early intervention and proper management can help improve symptoms, prevent complications, and enhance overall quality of life.
Varicose Veins Prevention in Nurses
Preventing varicose veins in nurses, who often spend long hours on their feet, involves adopting certain lifestyle habits and making changes to their work environment. Here are some preventive measures:
- Regular Exercise: Nurses should engage in regular physical activity to improve blood circulation in their legs. Walking, swimming, or cycling are excellent choices that promote leg movement and help prevent blood from pooling in the veins.
- Maintain a Healthy Weight: Excess weight puts additional pressure on the veins in the legs, increasing the risk of varicose veins. Nurses should strive to maintain a healthy weight through a balanced diet and regular exercise.
- Elevate Legs During Breaks: Taking short breaks during shifts to elevate the legs can help reduce pressure on the veins and prevent blood from pooling. Whenever possible, nurses should try to raise their legs to a level above the heart for 15-20 minutes.
- Avoid Prolonged Sitting or Standing: Nurses should avoid staying in the same position for long periods. If their job requires prolonged standing, they can shift their weight from one leg to another or take short sitting breaks when feasible.
- Wear Compression Stockings: Wearing graduated compression stockings can help support the veins and improve blood flow back to the heart. These stockings apply the most pressure at the ankles and gradually decrease pressure up the legs.
- Comfortable Footwear: Wearing comfortable, supportive footwear with proper arch support can alleviate pressure on the legs and reduce the risk of varicose veins.
- Stay Hydrated: Drinking an adequate amount of water throughout the day can help maintain good blood circulation.
- Avoid Crossing Legs: Crossing the legs can impede blood flow in the veins. Nurses should try to avoid sitting in positions that restrict blood circulation.
- Move and Stretch: Nurses can incorporate small movements and leg stretches during their shifts to keep the blood flowing and prevent stagnation.
- Work Environment Ergonomics: Hospitals and healthcare facilities can take steps to improve the working conditions for nurses. This includes providing anti-fatigue mats or padded flooring in areas where nurses stand for extended periods. They can also encourage rotating workstations to allow nurses to sit for some tasks.
Best Compression Socks for Nurses to Wear to Prevent Varicose Veins
It’s important for nurses and healthcare workers to be aware of the risk factors and symptoms of varicose veins. If any concerns arise or symptoms are experienced, they should seek medical advice for proper evaluation and management.
If you are a floor nurse, you spend hours on your feet every day. Standing and walking on cement can cause various leg conditions such as:
- Swelling
- Varicose veins
- Fatigue
It is important to wear quality compression socks to support your legs.
The ideal stockings should have at least 15-20 mmHg and they should be knee-high’s.They are the best compression stockings for nurses.
Almost 20% of the population will experience varicose veins. Varicose veins can occur:
- Varicose veins can occur in the groin
- Varicose veins can occur in the back of the knee
- Varicose veins can occur in the eyes
- Varicose veins can occur in the feet
- Varicose veins can occur in the upper thigh
- Varicose veins can occur in pregnancy
Quality compression socks prevent nurses from having leg fatigue. The following are the best compression socks for nurses
Compression stockings or anti-embolism socks are used for venous and lymphatic support. There are many forms of compression socks. These include:
Graduated or Medical Compression Socks
Best Compression Stockings to Prevent Blood Clots
- Anti-embolism socks are used to reduce the risk of deep vein thrombosis in nurses
- Like graduation compression socks, they provide gradient compression
- They are designed for bedridden patients and do not meet the technical specifications for use by ambulatory patients
- Although the terms “anti-embolism socks” and “graduated compression hosiery” are often used interchangeably and both types of stockings offer graduated compression, they have different levels of compression and indications
They usually exert considerably less compression than graduated compression socks.
They can often be bought over the counter without a prescription
These are the type of stockings that nurses need to wear to prevent varicose veins and spider veins.
Nurses stand on their feet all day. Especially nurses that work in the operating room. This can lead to swelling and pooling of the blood.
This is a perfect storm for blood clots or deep vein thrombosis in the legs. Compression stockings are able to increase blood flow, and this will increase circulation.
Also, for nurses who already have edema in their legs, compression stockings can help because they prevent the tissue in the legs from expanding.
Poor blood circulation and insufficient venous circulation are the main causes of varicose veins. Sometimes the valves in the veins do not let blood flow adequately.
This will cause the veins to bulge, this budges is known as spider veins or varicose veins. When a nurse wears compression stockings, the blood is forced back up to the heart and this will prevent varicose veins.
Nurses work extremely hard, oftentimes with no support resources. Patients are getting sicker and nurses are expected to work harder without increased support. This puts a lot of wear and tear on the nurses’ legs, joints, and back. One of the ways to prevent pain is to wear compression stockings.
Conclusion
The prevention of varicose veins in nurses is important because varicose veins hurt. I have seen nurses have to end their careers. Compression stockings can prevent varicose veins in nurses.


